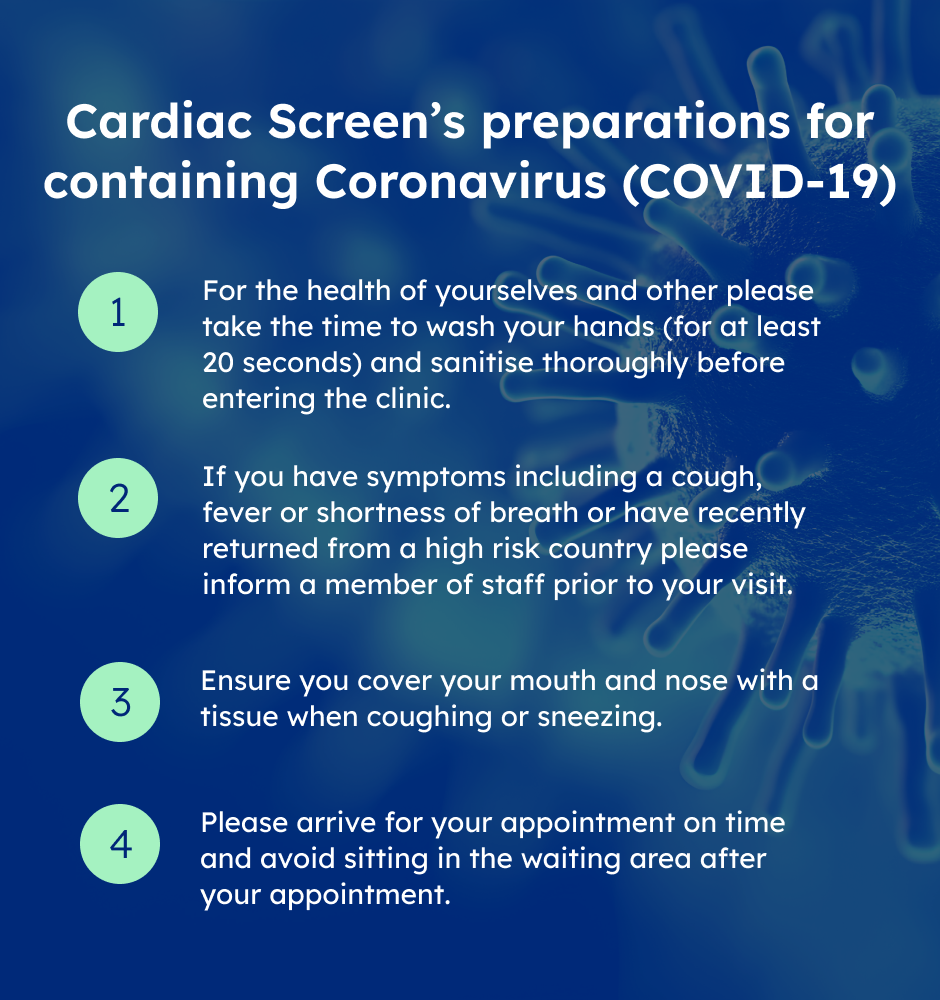
Please click here to view Cardiac Screen's preparations for containing Corona Virus
Balppa House, 57-61 Newington Causeway, London SE1 6BD
Gynaecology Services
Meet Our Medical Specialists
When to have a Gynaecology screening
A gynaecology screeningis recommended for annual screening for all age group of women and any time a woman has concerns about symptoms such as pelvic, vulvar, and vaginal pain, or abnormal bleeding from the uterus.
Conditions commonly treated by gynecologists include:
- Issues relating to pregnancy, fertility, menstruation, and menopause
- Family planning, including contraception, sterilization, and pregnancy termination
- Problems with tissues that support the pelvic organs, including ligaments and muscles
- Sexually transmitted Infections(STIs)
- Polycystic ovary syndrome
- Urinary and fecal incontinence
- Benign conditions of the reproductive tract, for example, ovarian cysts, fibroids, breast disorders, vulvar and vaginal ulcers, and other non-cancerous changes
- Premalignant conditions, such as endometrial hyperplasia, and cervical dysplasia
- Cancers of the reproductive tract and the breasts, and pregnancy-related tumors
- Congenital abnormalities of the female reproductive tract
- Emergency care relating to gynecology
- Endometriosis, a chronic condition that affects the reproductive system
- Pelvic inflammatory diseases, including abscesses
- Sexuality, including health issues relating to same-sex and bisexual relationships
- Sexual dysfunction
Gynaecology tests include:
- Transvaginal /Transabdominal Ultrasound
- Vaginal Swabs
- Smear tests
- Hormonal Blood profile
- Tumour markers
- Routine blood tests
- Urine test
- Mammogram