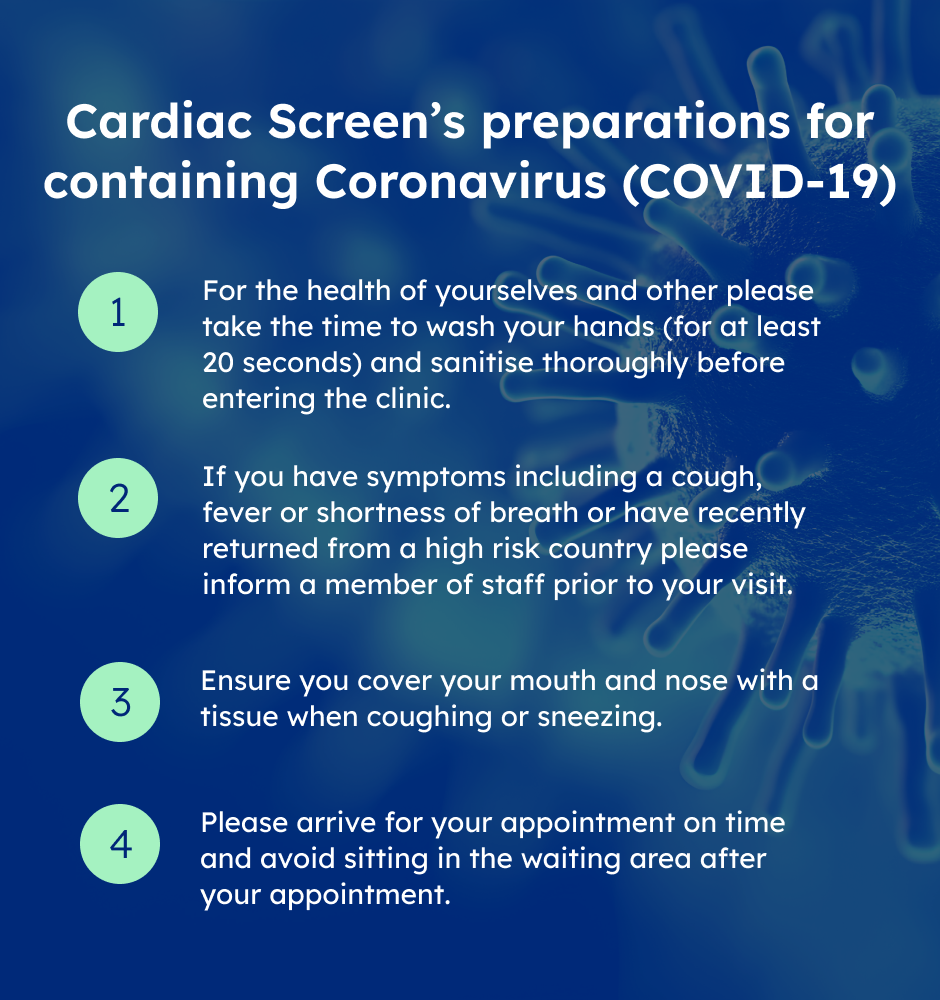
Please click here to view Cardiac Screen's preparations for containing Corona Virus
Balppa House, 57-61 Newington Causeway, London SE1 6BD
FAQs
Meet Our Medical Specialists
FAQs
Please click on the questions below to find the answer
An electrocardiogram (ECG) is a very quick and painless test that records the electrical activity of the heart. It is used to assess the rate and regularity of heartbeats, the size and position of the chambers, the presence of any damage to the heart and the effects of drugs or devices used to regulate the heart (such as a pacemaker).
If you have no symptoms of illness, you simply make an appointment with us. Otherwise, you will need to ask your GP to refer you.
ECGs at Healthcare Now are performed by practitioners, specialists in the field.The equipment they use is at the very forefront of technology, giving you the comfort of knowing that you are in the best possible hands.
You will need to speak to your insurers to establish this.
Generally, there are no risks associated with an ECG. The equipment monitors the electrical impulses from your heart, it doesn’t emit electricity.
No. It’s a totally painless procedure.
About 10 minutes.
A report will be sent directly to your referring Doctor who will then communicate them to you.
Increasing Age
Male Sex (Gender)
Heredity (Including Race)
Male Sex (Gender)
Heredity (Including Race)
Tobacco Smoke
High Blood Cholesterol
High Blood Pressure
Physical Inactivity
Obesity and Overweight
Diabetes Mellitus
High Blood Cholesterol
High Blood Pressure
Physical Inactivity
Obesity and Overweight
Diabetes Mellitus
Stress
Alcohol
Alcohol
Increasing age — Over 83 percent of people who die of coronary heart disease are 65 or older. At older ages, women who have heart attacks are more likely than men are to die from them within a few weeks.
Male sex (gender) — Men have a greater risk of heart attack than women do, and they have attacks earlier in life. Even after menopause, when women's death rate from heart disease increases, it's not as great as men's.
Heredity (including Race) — Children of parents with heart disease are more likely to develop it themselves. African Americans have more severe high blood pressure than Caucasians and a higher risk of heart disease. Heart disease risk is also higher among Mexican Americans, American Indians, native Hawaiians and some Asian Americans. This is partly due to higher rates of obesity and diabetes. Most people with a strong family history of heart disease have one or more other risk factors. Just as you can't control your age, sex and race, you can't control your family history. Therefore, it's even more important to treat and control any other risk factors you have.
Tobacco smoke — Smokers' risk of developing coronary heart disease is 2–4 times that of nonsmokers. Cigarette smoking is a powerful independent risk factor for sudden cardiac death in patients with coronary heart disease; smokers have about twice the risk of nonsmokers. Cigarette smoking also acts with other risk factors to greatly increase the risk for coronary heart disease. People who smoke cigars or pipes seem to have a higher risk of death from coronary heart disease (and possibly stroke) but their risk isn't as great as cigarette smokers'. Exposure to other people's smoke increases the risk of heart disease even for nonsmokers.
High blood cholesterol — As blood cholesterol rises, so does risk of coronary heart disease. When other risk factors (such as high blood pressure and tobacco smoke) are present, this risk increases even more. A person's cholesterol level is also affected by age, sex, heredity and diet.
High blood pressure — High blood pressure increases the heart's workload, causing the heart to thicken and become stiffer. It also increases your risk of stroke, heart attack, kidney failure and congestive heart failure. When high blood pressure exists with obesity, smoking, high blood cholesterol levels or diabetes, the risk of heart attack or stroke increases several times.
Physical inactivity — An inactive lifestyle is a risk factor for coronary heart disease. Regular, moderate-to-vigorous physical activity helps prevent heart and blood vessel disease. The more vigorous the activity, the greater your benefits. However, even moderate-intensity activities help if done regularly and long term. Exercise can help control blood cholesterol, diabetes and obesity, as well as help lower blood pressure in some people.
Obesity and overweight — People who have excess body fat — especially if a lot of it is at the waist — are more likely to develop heart disease and stroke even if they have no other risk factors. Excess weight increases the heart's work. It also raises blood pressure and blood cholesterol and triglyceride levels, and lowers HDL ("good") cholesterol levels. It can also make diabetes more likely to develop. Many obese and overweight people may have difficulty losing weight. But by losing even as few as 10 pounds, you can lower your heart disease risk.
Diabetes mellitus — Diabetes seriously increases your risk of developing cardiovascular disease. Even when glucose levels are under control, diabetes increases the risk of heart disease and stroke, but the risks are even greater if blood sugar is not well controlled. From two-thirds to three-quarters of people with diabetes die of some form of heart or blood vessel disease. If you have diabetes, it's extremely important to work with your healthcare provider to manage it and control any other risk factors you can.
Stress — Individual response to stress may be a contributing factor. Some scientists have noted a relationship between coronary heart disease risk and stress in a person's life, their health behaviors and socioeconomic status. These factors may affect established risk factors. For example, people under stress may overeat, start smoking or smoke more than they otherwise would.
Alcohol — Drinking too much alcohol can raise blood pressure, cause heart failure and lead to stroke. It can contribute to high triglycerides, cancer and other diseases, and produce irregular heartbeats. It contributes to obesity, alcoholism, suicide and accidents. The risk of heart disease in people who drink moderate amounts of alcohol (an average of one drink for women or two drinks for men per day) is lower than in nondrinkers. One drink is defined as 1-1/2 fluid ounces (fl oz) of 80-proof spirits (such as bourbon, Scotch, vodka, gin, etc.), 1 fl oz of 100-proof spirits, 4 fl oz of wine or 12 fl oz of beer. It's not recommended that nondrinkers start using alcohol or that drinkers increase the amount they drink.
Based on the definition from the Canadian Association of Cardiac Rehabilitation Cardiac Rehab is: "...the enhancement and maintenance of cardiovascular health through individualized programs designed to optimize physical, psychological, social, vocational, and emotional status. This process includes the facilitation and delivery of secondary prevention through heart hazard identification and modification in an effort to prevent disease progression and recurrence of cardiac events. Reference: The Canadian Association of Cardiac Rehabilitation - Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention First Edition, 1999.
Anyone who has a history of:
-
A heart attack
-
Bypass surgery
-
Angioplasty
-
Angina
-
Congestive heart failure
-
Is high risk for coronary artery disease
-
Heart transplant
-
Improves exercise tolerance and strength
-
Reduces blood fat levels
-
Improves angina and shortness of breath
-
Improves blood pressure
-
Improves blood glucose control
-
Improves psychological well-being
-
Improves quality of life
-
Speeds ability to return to work
-
Increases awareness of cardiac risk factors
-
Reduces stress
-
Decreases the incidence of cardiovascular disease
-
Reverses the effects of heart disease
-
Reduces hospital readmission rates
-
Reduces death rate by up to 24%
-
Provides safe and cost-effective treatment, when compared with other therapies
Yes. Those who are overweight, smoke, have high blood pressure or diabetes, abnormal risk test results, and those with a family history of heart disease are at greater risk.